Hip adductor tendinopathy (HAT) describes a series of conditions that develop in and around the tendon in response to chronic overuse of the tendon. At the histopathological level, changes occur in the molecular structure of the tendon, typically collagen separation and degeneration, and at the macroscopic level, tendon thickening, loss of mechanical properties and pain are usually observed. The role of inflammation is increasingly being questioned as studies have shown that there are no inflammatory cells around the affected area, making the term "tendinitis" obsolete.
Clinically Relevant Anatomy
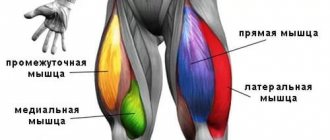
The adductors of the thigh consist of 5 muscles that can be divided into long (gracilis and adductor magnus) and short (pectineus, adductor brevis and adductor longus) adductors. These muscles help stabilize the pelvis and bring the hips toward the midline.
The adductor muscles originate from the lower part of the pelvic bone and attach to the femur, located between the hip flexors and extensors. They are used when we cross our legs, or, more importantly, when balancing the pelvis while standing and walking.
The adductor magnus is the largest muscle of this group, located behind all the others. There are 2 parts of this muscle - a part that functionally belongs to the adductors and a part that belongs to the hamstrings. The adductor portion extends from the inferior ramus of the pubis and the ramus of the ischium, attaching to the linea aspera of the femur and the medial epicondyle (to its tendinous attachment). The part related to the hamstrings extends from the tuberosity of the ischium to the adductor tubercle and the medial supracondylar line. The function of the adductor magnus muscle is adduction, assisting in hip flexion (adductor part) and hip extension (hamstring part).
In order not to miss anything interesting, subscribe to our Telegram channel.
The adductor longus muscle extends from the superior ramus of the pubis and the pubic symphysis and inserts into the linea aspera of the femur. It is a large and flat fan-shaped muscle that forms part of the medial border of the femoral triangle. It also forms an aponeurosis at its distal insertion, which extends to the vastus medialis muscle. The adductor longus muscle adducts and medially rotates the thigh.
The adductor brevis muscle is located under the long muscle and extends from the inferior ramus of the pubis to the posterior part of the linea aspera of the femur. The short muscle adducts the thigh.
The gracilis is a single biarticular muscle, extending from its insertion on the inferior border of the symphysis pubis to the medial surface of the tibia, inserting into the pes anserine between the tendons of the sartorius and semitendinosus. It is the most superficial muscle of the adductor group, whose function is to adduct the hip and flex the knee.
Human thigh: where it is located, anatomy, topography, structure of the lower leg (muscles, bones, blood vessels)
The structure of the femur is significantly different from others. This is due to the fact that it has the largest diameter among all tubular bones and is the longest in the body. It makes up the proximal part of the lower limb and is directly involved in moving the body.
Structures that make up bone tissue
The upper end of the femur ends with the head. Due to it, the limbs come into contact with the acetabulum, and thanks to the rounded shape of this formation, such an extensive range of movements is possible.
The connection of the head with the rest of the bone is at an obtuse angle, and is a neck.
On the bone itself there are many protrusions and depressions that correspond to the places of attachment of muscles and ligaments, vessels and nerves running here.
Muscular system of the thigh
The largest muscle in the human body is called the quadriceps, and is located in the lower limbs.
The structure of the hip. The femur is covered by many muscles, among the main ones the following groups can be distinguished:
- Flexors - located on the anterior surface of the limb. These include: quadriceps;
- tailoring;
- straight;
- lateral, medial and intermediate.
- Extensors – located along the posterior axis of the thigh and are represented by the following muscles:
- common tendon;
- semitendinosus;
- semimembranous;
- The inner group is located under the outer layer. It includes the following muscles:
- comb;
- long, magnus and short adductor.
- It is limited superiorly by the inguinal ligament.
- Above and behind - the gluteal ligament.
- Below - a line that can be drawn 5 cm above the patella.
Limb vessels
The blood supply is carried out by the femoral artery, which is a fairly large vessel originating from the external iliac, and that, in turn, from the aorta. Superficial and deep branches extend along it, feeding the soft tissues of the legs. Behind the thigh, the arterial vessels are close to the surface and therefore, when wounded, severe bleeding occurs.
Nerve bundle
The femur is innervated by its own saphenous nerve. In turn, it is divided into a cutaneous and a muscular branch in the area of the groin ligament. This complex system is connected together with the vessels and makes up the femoral bundle. In addition, the sciatic nerve runs along the back surface of the limb. It reaches the popliteal fossa, sending out small branches.
What is a hip?
The thigh (lat. femur) is the proximal component of the human lower extremities, located between the hip and knee joints. Its presence is also typical for other mammals, birds, and insects.
The anatomy of the human hip is as follows:
To understand that this is a hip, let’s thoroughly analyze its structure.
Femur injuries
Often the femur undergoes fractures. In this case, the integrity of the bone elements is disrupted, and the fragments injure the neurovascular bundles, causing severe bleeding, painful shock and dysfunction of the limb. More often, bone splitting occurs in the neck or soft tissues surrounding the joint. This is due to the structural features of the bone.
Restoring limb function after injury takes a long time and can last for years.
Anterior muscles
Let's look at the anterior muscle group.
| Muscle name | Task | Origin of muscle | Attachment |
| Quadriceps: wide intermediate, straight, wide medial, wide lateral. | Extension of the hind limb at the knee joint. The rectus muscle has its own separate function - bending the limb at the hip joint to an angle of 90 degrees. | Intermediate: intertrochanteric femoral line. Lateral: intertrochanteric vector, greater trochanter, lateral lip of the broad femoral line. Medial: medial lip of the rough femoral line. Straight: supraacetabular groove, iliac anterior inferior spine. | Tubercles of the tibia, medial part of the kneecap. |
| Tailoring | Bend the leg at the knee and hip joint, rotate the thigh outward and the shin inward. | Iliac anterior superior spine. | Tibial tubercles, intertwined with the crural fascia. |
Let's move on to the next large muscle group.
Diagnosis and treatment of injuries
To identify a hip fracture, an x-ray is done. To clarify the nature of the damage, computed tomography is used. In the first hours after the injury, the patient is given a splint or plaster cast.
This will prevent the injury from worsening during transport. Subsequent treatment is carried out using skeletal traction. Surgery is used to reposition bone fragments. Another treatment method is osteosynthesis.
It consists of implanting a metal or titanium plate.
Medial muscles
Let us now turn our attention to the medial group of the thigh muscles.
| Muscle name | Task | Origin of muscle | Attachment |
| Pectineus muscle | Bend the limb at the hip joint with simultaneous adduction and external rotation. | Upper branch of the pubic bone, pubic crest. | The pectineus muscle is attached to the upper part of the femur: between the rough surface and the back of the lesser trochanter. |
| Adductor major | Adduction, hip rotation, extension. | Inferior branch of the pubis, ischial tuberosity, branch of the ischium. | Rough part of the tubular bone. |
| Adductor long | Adduction, flexion, external rotation of the hip. | Outer part of the pubic bone. | Median lip of rough femoral vector. |
| Adductor short | Adduction, external rotation, hip flexion. | Outer bodily surface, lower branch of the pubic bone. | Rough hip bone vector. |
| Thin | Adduction of the abducted limb, participation in flexion of the knee joint. | The lower branch of the pubic bone, the lower part of the pubic symphysis. | Tubercles of the tibia. |
And finally, let's get acquainted with the last muscle group of this part of the body.
Nervous structure
The vast majority of nerve endings in the legs originate from the lumbar plexus. Therefore, when its integrity is violated, many complain about the muscles of the hip and knee flexion functions. There are two main nerves of the thigh - deep and femoral. Then they branch along the lower limbs, forming their own web, part of which will be, for example, the external cutaneous nerve of the thigh.
The femoral nerve passes through the back and outer part of the thigh, the pelvis. The obturator also follows through the pelvic area, but extends into the inner femoral surface.
The sacral nerve plexus, which forms under the piriformis muscle, also in the pelvis, is also important. Through the gluteal fold it descends to the posterior region of the thigh to then divide into the tibial and peroneal nerves.
What type of bone tissue is there?
Long or short, large or small, all bones are composed of tissue that can be reticulofibrous or lamellar.
The first is necessary for connection with the tendons. Thanks to lamellar tissue, almost the entire skeleton is provided with bone substance.
Its peculiarity is the presence of microscopic plates lying parallel to each other. The greater strength of the skeleton is due to the arrangement of the plates forming a right angle.
Additional strength is provided by the periosteum. Blood vessels, nerve nodes, and lymphatic vessels became part of it.
Source: https://ocrb.ru/problemy/bolshoj-vertel.html
Etiology
The hip adductors are active in many sports such as running, football, horse riding, gymnastics and swimming. The repetitive nature of the movements in some of these sports and the constant changes in direction place increased demands on the adductor tendons. This makes athletes more vulnerable to developing TPMB as well as groin pain. Other causes may include overstretching the hip adductor tendons or a sudden increase in the number or intensity of exercise.
The development of TPMB depends on many reasons. One such factor is significant leg length discrepancy, which affects gait pattern (although there is no explanation as to what is significant). Poor or altered movement patterns during physical activity can also put excessive strain on the hip adductor tendons. Differences in muscle length, strength imbalances, or muscle weakness in the lower extremity can also influence the development of tendinopathy. Other factors may include lack of warm-up, physical inactivity, fatigue, excess body weight, degeneration or genetics.
The structure of the human thigh
The anatomy of the human femur involves the study of muscle attachments, function, as well as trophic support - the localization of blood vessels and nerves. The performance of the lower limb depends on the condition of the lumbar vertebrae and pelvic muscles.
The thigh is the upper part of the lower limb, the area between the pelvis and the knee. The muscles passing through this area control the hip and knee joints, therefore they are called two-joint:
- The volume of the front part and strength of the thigh is given by the quadriceps muscle - the main extensor of the knee. For example, when walking or when playing football. She also performs flexion at the hip joint.
- A group of flexors runs along the back, which has other functions in relation to the pelvic region - it promotes extension.
Therefore, the hip bones form two large joints of the lower limb.
Where is it located and what does it consist of?
The photo shows that the thigh is limited by the inguinal ligament in front and the gluteal folds in the back. The area ends 5 cm above the knee.
It includes the longest bone, which forms two joints - the knee and hip. Contraction of the thigh muscles is provided by nerves from the lumbar plexus.
Next to them lie arteries that supply blood to bones, muscles, and skin. Veins take blood, providing outflow from the lower extremities. Trophic supply passes through the tendon canals. The thigh area contains lymph nodes and blood vessels.
Clinical picture
TPMB is usually felt as pain in the groin when palpating the adductor tendons, adductor and/or the injured leg. The pain may develop gradually or appear as a sharp, sharp pain.
You may also experience swelling or tightness in the adductor muscle(s), stiffness in the groin area, or an inability to contract or stretch the adductor muscles. In severe cases, exercise will be limited as the tendon can no longer withstand repeated stress.
Arteries and vessels
Arterial vessels participate in the blood supply to the zone:
- Femoral (superficial). It is a continuation of the external iliac. In the area of the femoral triangle, the superficial epigastric branch departs from it (directs upward, to the lower abdomen).
- Obturator – goes around the ilium, nourishes the groin area.
The first branches in the area of the femoral triangle. Branches extend from it:
- external genitalia - supply blood to the genitals;
- deep – placed 3-4 cm below the groin, running along the back of the thigh;
- medial (superficial, going down, stretches between the long and short adductors; deep, separating the iliopsoas and pectineal);
- lateral – surrounds the femur, is located under the rectus muscle, creates an ascending and descending branch;
- piercing - stretch behind the thigh.
The vessels of the thigh supply the entire limb, the lower abdomen.
Prevention
To prevent the development of TPMB, an athlete must continually work on factors such as strength and coordination. At the same time, he must comply with all the requirements for recovery and adaptation in the intervals between training sessions.
The athlete must develop muscle strength to maintain pelvic stability through specific exercises that are appropriate to the demands of their activity/sport and have varying levels of difficulty (eg, speed training and jumping). Another important aspect is muscle flexibility. Regular stretching is recommended.
Treatment
Drug treatment
Pain management is recommended first, although NSAIDs may not be effective due to the non-inflammatory nature of the injury. Steroid injections are not always indicated due to the potential for tendon damage (if they are injected directly into the tendon).
Physical therapy
Physical therapy is recommended for the treatment of TPMB. Active therapy through an exercise program is superior to a more passive treatment approach. Recovery varies greatly between individuals as the disease can be degenerative. In general, patients may respond well to rehabilitation programs, but in some cases the tendon may be refractory to a range of treatments.
Strengthening the abdominal muscles is recommended to support the adductors during exercises as well as hip flexion exercises. Exercises should be tailored to the specific sport to avoid recurrence of injury. In most cases, return to normal function can occur within a few weeks, but in more severe cases, rehabilitation may take several months to return to normal, pain-free activity.
Diagnosis and treatment
If you have injured the hip area and you suspect the development of pathology, you should contact an orthopedic specialist. Diagnostics consists of examination, palpation, and then analysis and instrumental methods - x-rays, tomography, angiography, electromyography, etc.
Treatment methods depend on the severity of the disease, the age of the patient, and the nature of the pathology. At the beginning, therapy is conservative - splint, plaster, medications, massage, physiotherapy, gymnastics. If this complex does not lead to a satisfactory result, the hip joint is replaced with an artificial one during surgery.
Lead tactics
Rest is necessary for the first 48 hours after injury. Apply the RICE concept (rest, ice, compression and elevation) 3 times daily for 10-20 minutes to help reduce swelling and inflammation. Once the swelling has subsided, blood flow stimulation therapy can be started to enhance the healing process. Active treatment is then indicated to maximize rehabilitation. Its goal is to restore the properties of muscles and tendons, since strength training has a beneficial effect on the structure of the tendon matrix, muscle properties and biomechanics of the limbs. Recent evidence suggests that an eccentric exercise program is most effective. You can also slowly perform eccentric and concentric exercises with heavy weights to improve pain and tendon function. However, Cook et al. proposed a new, 3-stage model of tendinopathy, where exercise treatment differs between stages. They suggest that the current treatment protocol of adding eccentric loading used for stages 2 and 3 may be detrimental to stage 1 tendinopathy. For effective treatment, staging the tendinopathy is critical.
Loading provides a positive stimulus to both tendon and muscle tissues, however there is no single effective method for tendon rehabilitation, with variations in repetitions, sets and load applied depending on the stage of rehabilitation and the patient's muscle-tendon response to training. The exercises are aimed at eliminating neuromuscular and tendon changes (strength and functional ability) associated with tendinopathy.
The stages suggested by Cook et al: reactive tendinopathy, tendon injury (failed healing) and degenerative tendinopathy. In the early, reactive stages, the key is to change the load to an acceptable level at which the tendon can repair and heal. Cook suggests, however, that the tendons may have a latent reaction for about 24 hours. This means that what appears to be non-reactive immediately after activity may flare up 24 hours later. At this stage, the use of non-steroidal anti-inflammatory drugs is not clear-cut, but it is believed that their use may be beneficial. Always consult your doctor before taking any medications.
Stretching is also not indicated during the reactive stage because it can place compressive stress on the affected tendon, worsening symptoms. One option is massage to maintain muscle length. In this acute stage, treatment with isometric exercises (instead of eccentric exercises) along with rest from excessive physical activity is recommended. Those. It is necessary to rest from activities, which may include parameters such as speed, distance and intensity, and to be cautious of any pain that may occur after 24 hours. Symptoms and pain response should be a guide, so cross-training is recommended to maintain fitness and function. At this stage, reverse changes in the tendon are possible.
Stage 2 tendinopathy is usually characterized by persistent discomfort with local thickening of the tendon from chronic overuse and can occur in patients of different ages depending on the duration of exposure, frequency and intensity of loading. Stage 2 may be difficult to discern clinically.
In stage 3 degenerative tendinopathy, cellular and matrix changes progress to irreversible levels, so treatment is focused on the long term, which includes eccentric loading as well as strengthening and stabilization exercises. Degenerative tendon is usually seen in older athletes and sometimes in younger ones depending on the degree of chronic overload. There may be areas of thickening, and acute attacks of pain may indicate areas of stage 1 tendinopathy. If the tendon is severely degenerated, there is a risk of rupture. Therefore, treatment should address symptoms according to stage 1 until the acute pain subsides, followed by a long-term exercise program.
Malliarus et al. suggest that there is little evidence to highlight the eccentric component in the rehabilitation of Achilles tendinopathy and patellar tendinopathy. In their opinion, a rehabilitation program that includes eccentric, concentric and isometric exercises gives the best results.
There is more than one way to treat tendinopathy, so it is recommended to work with a physical therapist to manage symptoms, and to use rest along with a gradual return to activity. Once symptoms resolve, a gradual return to normal stretching is possible. However, stretching should never cause pain.
Here are some examples of hip adductor stretches:
- Adductor brevis: Sit in a position as shown below (avoid slouching in the lower back);
- Gently press your elbows toward your knees until you feel a stretch in the muscles;
- hold in this position for 20-30 seconds, repeat 3-4 times.
Stretching the short adductor muscles
- Long adductor muscles: stand and spread your legs into a wide stance;
- bend the opposite knee, leaning in the same direction until you feel a stretch;
- hold this position for 20-30 seconds, repeat 3-4 times.
Long adductor muscle stretch
Examples of exercises
An example of an isometric exercise: sit on a chair with an elastic band located above the knee and keep your leg in an adducted position (against the resistance of the elastic band); hold this position as long as it is comfortable; The resistance can be adjusted by stretching the band more or less.
An example of an exercise that strengthens the adductor muscles of the thigh: stand near a table with an elastic band located on the lower leg; stand on the step platform with your healthy leg so that the affected leg can swing freely; Keeping your back and knee straight, slowly move your leg away from the midline, then bring your leg down.